
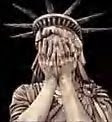
Undocumented Immigrants draining the social services. Sounds familiar to you. Then Someone Lie to you.
MISSOURI HEALTH CARE SYSTEM TO PAY U.S. $60 MILLION TO SETTLE FALSE CLAIMS ACT ALLEGATIONS.
WASHINGTON – Lester E. Cox Medical Centers, a health care system headquartered in Springfield, Mo., has agreed to pay the United States to settle claims that it violated the False Claims Act, the Anti-Kickback Statute and the Stark Statute between 1996 and 2005, by entering into certain financial relationships with referring doctors at a local physician group and engaging in improper billing practices with respect to Medicare. Cox, a not-for-profit healthcare organization, will pay the United States $60 million to resolve these claims.
Under the Stark Statute, Medicare providers like Cox are prohibited from billing the federal health care program for referrals from doctors with whom the providers have a financial relationship, unless that relationship falls within certain exceptions. The United States contended that certain relationships between Cox and physicians ran afoul of the Anti-Kickback Statute, which prohibits offering inducements to providers in return for patient referrals, and the Stark statute. Additional claims being resolved concern Cox’s inclusion of non-reimbursable costs on its Medicare cost reports and improper billings for services provided to dialysis patients.
“The Justice Department is committed to ensuring that the best interests of federal health care program patients are not compromised by unlawful payments to physicians,” said Gregory G. Katsas, Assistant Attorney General for the Justice Department’s Civil Division. “The resolution of this matter resulted in a significant recovery for taxpayers, and it exemplifies our dedication to vigorous enforcement of the Stark and Anti-Kickback Statutes.”
As part of the $60 million settlement, Cox has entered into a Corporate Integrity Agreement with the U.S. Department of Health and Human Services (HHS) Office of Inspector General. The Corporate Integrity Agreement contains measures to ensure compliance with Medicare regulations and policies in the future.
“Today’s settlement furthers both our commitment to protecting patients from improper billing practices and the continued ability of Cox to provide quality medical care in Springfield and the Ozarks,” said John F. Wood, U.S. Attorney in Kansas City, Mo. “I am pleased that we were able to resolve this matter without litigation.”
The settlement with Cox was the result of a coordinated effort by the Commercial Litigation Branch of the Justice Department’s Civil Division; the U.S. Attorney’s Office for the Western District of Missouri; HHS’ Office of Inspector General, Office of Counsel to the Inspector General, and Office of Audit Services; and the FBI


No comments:
Post a Comment